The endometrium is triangular and continuous, in its upper corners, with the lumina of the fallopian tubes and the cervix at it lower point.
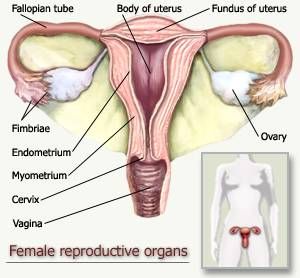
Figure 1: Diagram of the Female Reproductive Tract.
The endometrial lining is composed of columnar epithelial cells supported by a cellular stroma with tubular glands.
Figure 2: Endometrial Tissue Composed of Columnar Epithelia, Stroma and Tubluar Glands(Arrows).
The uterine mucosa is composed of the isthmus and corpus. The isthmus is thin mucosa and is not very responsive to hormonal stimuli; it is located between the endometrium and the endocervix in the lower portion of the uterine cavity. The corpus (endometrium) is a mucosa which is fully responsive and affected by female hormonal stumuli and their cyclic fluctuations. The corpus itself can be divided into two layers: the lower layer known as the basalis and the upper layer known as the functionalis.

Figure 3: Diagram of the Female Uterus in Order to Highlight the Isthmus and the Corpus of the Endometrium.
The basalis is the zone of relative inactivity adjacent to the myometrium of the uterus. The basalis is an area of weakly proliferative gland cells and dense spindle shaped stromal cells. It is known as the reserve cell layer and it is responsible for regenerating the endometrium after the functionalis has shed. Its thickness remains constant throughout the menstrual cycle. The functionalis is a region of proliferative glandular cells which are arranged in sheets due to the mutual adhesiveness between gland cells. Little proliferation of cells is shown in the early phases of the menstrual cycle; however as estrogen levels rise, proliferation is more apparent and in the late proliferatory phase, the epithelial layer changes to a pseudostratified or stratified columnar epithelium. Since the endometrial tissue is highly sensitive to female steroid hormone levels in the body, its composition undergoes many changes depending on a woman’s age and fertility.
Before Puberty: Estrogen and progesterone levels are low and the endometrium is atrophic showing a lack of mitotic activity in its gland it is similar to the endometrial state after menopause.
After Menopause: The endometrium is once again atrophic. The lining is thin and smooth. The glands are a single layer of flattened cuboidal cells and the stromal cells are spindled and closely packed.

Figure 4: Histological Section of an Atrophic Endometrium.
During the Reproductive Years: The endometrium is composed of:
• Glandular epithelia
• Proliferative glands
• Secretory glands
• Surface glandular epithelium
• Stoma
• Vasculature
The endometrial cells synchronously proliferate, differentiate and shed cyclically every 28 days in response to estradiol and progesterone changes in the female human body. This 28 day cycle is known as the Menstrual Cycle and is categorized into phases.
Proliferation Phase:
Days 1-14 of the cycle. This phase exhibits ovarian secreted, estradiol induced proliferation of stroma, gland cells and vasculature.
Days 1-4 mark the menstrual phase which will be discussed below.
Days 4-13: proliferation of the endometrial lining ensues. The functionalis tissues increase in thickness with an increase in gland cells, stroma and vasculature. The glands and blood vessels increase in size and number faster than the stroma, causing them to become coiled giving the arteries a characteristic spiral conformation. The stromal cells become enlarged by edema and an increase in glycogen content and pack closer together.
Secretory Phase:
Occurs after ovulation on day 14. Estradiol and progesterone secreted from the corpus luteum induce secretions and differentiation of stromal cells into predecidualized cells.
Days 14-28: secretions are noticed in the epithelial layer The endometrium is abundant with closely packed gland and enlarged glands. In late secretory phase, the stomal cells become predecidual and surround the spiral arteries. The secretions slow down and neutrophils and lymphocyte-like granulocytes infiltrate the stroma. These granulocytes are thought to release relaxin that dissolve reticular fibers found near the stromal cells just before endometrial shedding of the menstrual phase.
If implantation does not occur the menstrual phase progresses.
Menstrual Phase:
Days 1-4 Endometrial shedding takes place. Around the 28th day of the menstrual cycle, there is a sudden reduction in the thickness of the functionalis due to a decreased steroid hormone levels in the body. This causes impaired blood flow to the upper portion of the endometrium leading to ischemia, necrosis and hemorrhage of the endometrial lining. During this phase, there is an increase in leukocytes and fibrin thrombin appears in blood vessels in the area. The collapsed stroma, ruptured glands, neutrophils, granulocytes and ruptured vasculature is what is shed during this phase.

Figure 5: Diagram of Endometrial Thickness in Response to Hormonal Stimulation.
However if implantation does occur before shedding, there is a resurgence of gland secretions and exaggerated stromal decidualization where almost all endometrial stroma is converted to sheets of large decidual cells.
Cells of the Endometrium
-Ciliated glandular cells: more prominent near the isthmus, they are most apparent in the proliferative phase but still visible in the secretory phase. These cells occur most often in estrogen stimulated endometrial they are smaller than secretory cells and are columnar in palisading arrangements.
-Stromal cells: in early proliferative phase, they are undifferentiated fibroblast cells which are small and ovoid. They are loosely grouped or can appear singly in the tissue. As the menstrual cycle proceeds, the stromal cells become more fibroblast like, spindled and larger. Mid cycle these cells become grouped. During pregnancy these cells become enlarged.
Some Endometrial Pathologies:
Non specific endometritis: inflammation of the endometrium from an undetermined cause. Usually a variety of factors are associated with this form of inflammation such as:
-Disruption of the cervical mucous barrier
-Intrauterine necrosis
-Interruption of regular endometrial shedding
As the inflammation become more severe the entire corpus is inflamed including the basalis, this reaction interrupts the endometrium’s normal processes.
Endometrial Hyperplasia: Abnormal proliferation of endometrial cells; it can cause the endometrium to grow outside the uterus. These cells still respond to hormonal stimuli in the body and can cause endometrial tissue build up on organs outside the uterus.
Carcinoma of the endometrium: related to endometrial hyperplasia, it is a cancer of the endometrium. Usually the carcinoma is preceeded by severe hyperplasia in young women. It typically occurs in older females and in particular females with:
-Diabetes
-Obesity
-Infertility
-Late onset menopause
It is characterized by polyp-like malignant tumors on the surface of the endometrium. These tumors cause the uterus to expand and the uterine cavity to become blocked with tumors.
References:
Aplin, John D., Fazleabas, Asgerally T., Glasser. Stanley R. and Giudice, Linda C. (Editors) (2008) The Endometrium: Molecular, cellular and Clinical Perspectives. Informa Healthcare: London.
Buckley, C.H. and Fox, H. (2002) Biopsy Pathology of the Endometrium: Second Edition. Arnold: New York.
Tae, Liang-Che (1993) Cytopathology of the Endometrium: Direct Intrauterine Sampling. American Society of Clinical Pathologists: Chicago.
Figure 1: http://buttercuppunch.files.wordpress.com/2009/04/uterus.jpg
Figure 2 : http://www.kumc.edu/instruction/medicine/anatomy/histoweb/female/small/Fem12s.JPG
Figure 3 : http://www.apsu.edu/thompsonj/Anatomy%20&%20Physiology/2020/2020%20Exam%20Reviews/Exam%205/27-14a_Uterus_1.jpg
Figure 4 : http://www.hsc.stonybrook.edu/gyn-atlas/images/DSCN3423B.jpg
Figure 5 : http://image.tutorvista.com/content/reproduction-in-animals/menstrual-cycle-phases.jpeg
No comments:
Post a Comment
Note: Only a member of this blog may post a comment.